Although electricity has been used for centuries to treat pain & many other ailments, stimulation of dorsal column of spinal cord was first used by Shealy & his colleagues in 1967. Their study was based on the “Gate control theory of pain” by Melzack and Walls introduced in 1965. Initially they termed the procedure as dorsal column stimulation as they believed that stimulation is effective only at dorsal horn of spinal cord. As it is now known that electrical stimulation is effective in suppression of nociception when applied in almost anywhere of the spinal cord, so the better and more acceptable term is spinal �cord stimulation� by spinal cord stimulator.
Mechanism of action of spinal cord stimulation:
Spinal cord stimulator act in by several ways.
- Gate control theory of pain The pain impulses from periphery are transmitted through smaller diameter nonmyelinated C fibres and lightly myelinated A-delta fibres. They terminate at the substantial gelatinosa of dorsal horn of spinal cord (the gate). Other sensory impulses like touch and vibration are carried by larger diameter myelinated A-beta fibres that also terminate at the dorsal horn (gate) of spinal cord. The reception of large fibre information (touch and vibration) would switch off the gate to reception of small fibre information. The end result of this closure of gate is analgesia. Shealy and colleagues use same principle; stimulation of A-beta fibres of dorsal column by electricity closes the gate and antidromically inhibits the pain impulses from small fibres.
- It produces supraspinal inhibition of pain either by inhibiting pain transmission or modulation of pain impulses.
- Blocking transmission in the spinothalamic tract
- It activates the central inhibitory mechanisms for influencing sympathetic efferent neurons. This leads to vasodilatation. In fact this effect is used in improving perfusion in peripheral vascular disease and also to take care of pain.
- It has been observed that even after cessation of spinal cord stimulation, the analgesia lasts for longer time. This is being attributed to activation of putative neurotransmitters or neuromodulators.
Advantages:
This therapy aims at pain relief in patients who are refractory to all other treatment modalities. They are very tough group to get good results.
There are many advantages of using this therapy like:
- It’s a simple Percutaneous/ surgical procedure.
- It’s a nondestructive procedure. No permanent surgical or chemical interruption of nerve pathway is done.
- A trial therapy checks whether patient is going to get pain relief or not.
- The procedure is reversible; if patient is not relieved of his symptoms, the stimulator can be removed. There will not be any side effects.
- From patient’s point of view:
- Significant reduction in pain intensity
- Reduction in opioids or other drug intake
- Improvement of quality of life.
Selection criteria:
- The pain syndrome should be established & patient should have radiating pain.
- The conservative treatments have failed.
- Drug addiction/alcohol abuse should be ruled out.
- There should be no major.
- Trial stimulation should be successful.
Indications:
- Failed back surgery syndrome/ perineural fibrosis
- Adhesive arachnoiditis
- CRPS type I & CRPS type II
- Post herpetic neuralgia
- Peripheral neuropathy
- Phantom limb pain/stump pain
- Peripheral vascular insufficiency
- Angina
- Cerebral palsy
- Multiple sclerosis
Absolute Contraindications:
The major contraindications are same as mentioned for any procedure:
- Infection
- Anticoagulants/coagulopathy
- Previous surgery or trauma that obliterates spinal cord.
Relative contraindications
- Pacemaker in situ.
- Major psychiatric problem
- Spinal bifida
Disadvantages & complications:
There are certain disadvantages with respect to spinal cord stimulation.
- Cost is high compared to other treatment options although is cost-effective.
- Requires highly-efficient team.
- There may be some complications in rare occasions like lead migration, lead fractures, infection etc.
Preliminary steps:
- Evaluation of pain
- Psychiatric evaluation
- Patient education: about pre- and post-procedure plan and long-term management, cost effectiveness
- Planning of procedure.
Procedure
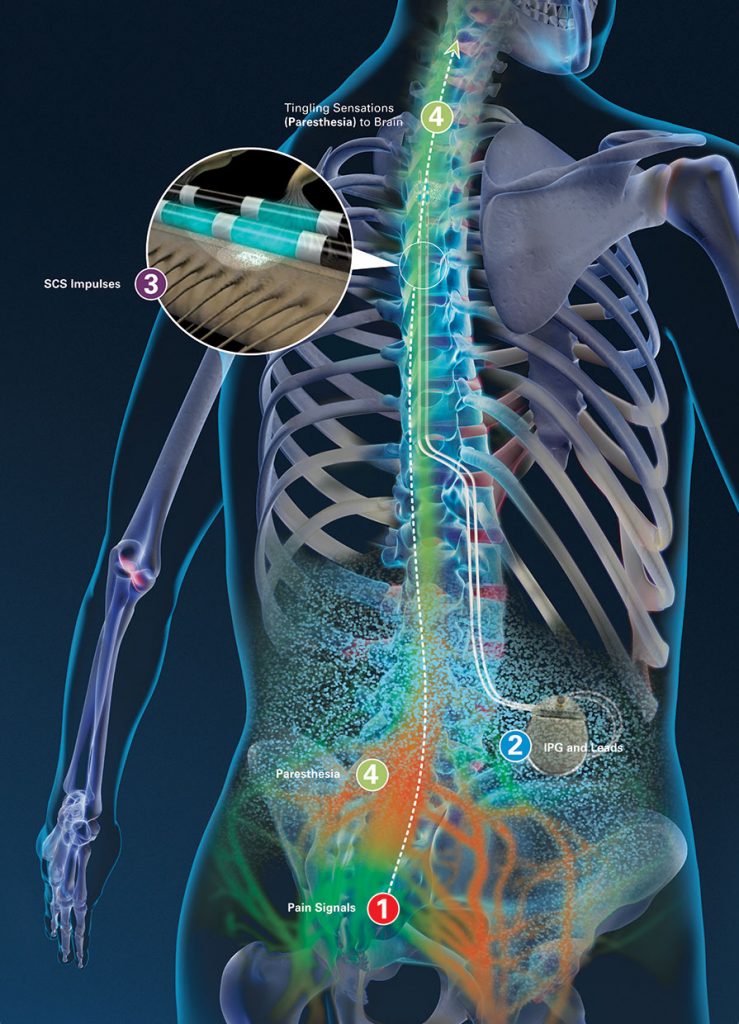
The procedure involves percutaneous insertion of lead, typically a “longitudinal” lead with a linear array of electrodes through an epidural needle into the epidural space and oriented parallel to spinal column. First step is the introduction of a trial electrode for temporary purpose. The lead is connected to an external battery source that transmits radiofrequency signals to the lead. The external transmitters help in adjusting the amplitude, pulse width and rate of stimulation. The low voltage electrical stimulation is applied to the spinal cord to create a current field that activates neurons in the dorsal column. This stimulation is done by the external power supply connected to lead by either a conducting wire or extension. The stimulation produces paraesthesia that interferes with or blocks pain signals to brain. The vertebral level at which it is placed depends upon the location of pain. If patient gets 50% or more pain relief after trial stimulation, then patient is considered for permanent implant. Replacing the temporary lead with permanent lead usually does this. Implanted pulse generator provides the power supply.
FAQ of Spinal Cord Stimulation
